Dealing with itchy eyes, a constantly runny nose, or sudden wheezing can really disrupt your life. Allergies and asthma often go hand-in-hand, making simple activities feel like huge hurdles. Understanding these conditions is the first step towards better control and finding relief through effective allergy and asthma care.
“You don’t outgrow asthma or allergies—they evolve. Effective care means adjusting your management plan as your life and environment change.”
Dr. Purvi Parikh
You are not alone if you find managing these symptoms confusing or frustrating. Millions face similar challenges daily, significantly impacting their well-being. This guide offers practical information and steps you can take for better allergy and asthma care, helping you breathe easier, live more comfortably, and focus on improving quality of life.
Understanding Allergies and Asthma
Grasping the basics of allergies and asthma helps you manage them better. They affect your body in different ways but are frequently linked through complex immune responses. Knowing the difference is important for getting the right diagnosis and appropriate asthma treatment or allergy care.
What Are Allergies?
Allergies occur when your immune system reacts to harmless substances. Your body mistakenly identifies these substances, known as allergens, as threats. It releases chemicals such as histamine. It also produces IgE antibodies. This causes allergy symptoms in different parts of the body.
Common allergens are airborne particles like pollen. They cause outdoor allergies or allergic rhinitis, also known as hay fever. Dust mites and mold spores are also common triggers.
Symptoms can vary. You may experience sneezing, itching, or hives (urticaria). Skin allergies, such as contact dermatitis, can happen. In severe cases, anaphylaxis may occur. Quick recognition and care are essential.
Allergies are a leading cause of chronic illness in the U.S., according to the American College of Allergy, Asthma & Immunology (ACAAI). Understanding various allergens and reactions is key to managing immunology health. To treat these conditions successfully, identify specific triggers and create a management plan.
What is Asthma?
Asthma is a long-term disease affecting the airways in your lungs. These airways become inflamed and narrowed, making it hard to breathe; this condition is often referred to as asthma asthma in some contexts to emphasize its chronic nature.
This inflammation makes the airways sensitive to various triggers, leading to recurrent symptoms. When exposed to a trigger, the airways swell, the surrounding muscles tighten, and the lining produces extra mucus.
This leads to symptoms like persistent coughing, wheezing (a whistling sound when breathing), shortness of breath, and chest tightness. Asthma severity varies greatly among individuals, ranging from mild intermittent symptoms to severe persistent asthma requiring intensive management from specialized asthma doctors.
The Allergy-Asthma Connection
Allergies and asthma are closely connected for many people, representing a significant area within clinical immunology. Allergic reactions can sometimes trigger asthma symptoms, a condition known as allergic asthma or allergy asthma.
The Asthma and Allergy Foundation of America (AAFA) notes this is the most common type of asthma, affecting a large portion of asthma sufferers1. Exposure to allergens like pollen, dust mites, mold, or pet dander can cause airway inflammation and constriction in susceptible people.
This directly leads to asthma attacks, demonstrating how intertwined these immunologic diseases can be. However, it is worth remembering that not all asthma is triggered by allergies; other factors like infections, exercise, cold air, or irritants can also play a significant role in triggering asthma symptoms.
Identifying Your Triggers
Knowing what sets off your allergy or asthma symptoms is crucial for effective management. Triggers can be different for everyone and may change over time. Identifying yours allows you to take steps to avoid them and prevent flare-ups.
Common Allergy Triggers
Allergens are everywhere, and identifying specific ones impacting you can require careful observation. Airborne allergens are frequent culprits for respiratory symptoms like allergic rhinitis. These include pollen from trees, grasses, and weeds (causing seasonal outdoor allergies), mold spores found in damp areas indoors and outdoors, tiny dust mites living in bedding, upholstery, and carpets, and proteins from pet skin flakes (dander), saliva, or urine.
Food allergies are another common issue, with substances like peanuts, tree nuts, milk, eggs, soy, wheat, fish, and shellfish often causing reactions ranging from mild itching to severe anaphylaxis. Careful food allergy testing and subsequent avoidance are necessary. For individuals following Ayurvedic principles, considering a Kapha diet may help balance the body and support overall well-being, especially when dealing with food sensitivities.
Other triggers can involve insect stings from bees, wasps, hornets, or fire ants, leading to venom allergy, and certain medications, which can cause drug allergy reactions. Keeping track of reactions helps pinpoint these specific causes for better patient care.
Common Asthma Triggers
Asthma triggers can overlap with allergy triggers but also include other factors that irritate the airways. Allergens like pollen, dust mites, mold, and pet dander are major asthma triggers for those with allergic asthma. But non-allergic triggers are also important to recognize and manage for comprehensive asthma care.
These include irritants in the air like tobacco smoke (firsthand and secondhand), air pollution from traffic or industry, wood smoke, chemical fumes from cleaning products or workplace exposures, and strong perfumes or scents. Respiratory infections, such as common colds, the flu, or sinusitis, are frequent triggers, especially in children.
Even physical activity (exercise-induced bronchoconstriction), exposure to cold, dry air, or strong emotional responses like stress or laughter can sometimes provoke asthma symptoms. Conditions like nasal polyps or eosinophilic esophagitis can also be associated with asthma.
How to Pinpoint Your Triggers
Figuring out your personal triggers often takes some detective work and collaboration with your health care provider. Keeping a detailed symptom diary can be very helpful for tracking patterns. Note when and where your symptoms occur, their severity, and what you were doing or exposed to beforehand, including foods eaten, activities, and environments.
Your doctor, potentially a board certified allergist, might recommend allergy testing to confirm suspected triggers. This testing is a cornerstone of allergy asthma care. Allergy skin testing, including skin prick testing (where tiny amounts of allergens are pricked onto the skin) or intradermal skin tests (injecting small amounts under the skin), can identify immediate allergic reactions2.
Patch testing is used to diagnose delayed reactions like contact dermatitis. Blood tests measuring specific IgE antibodies to allergens can also be useful, especially if skin tests cannot be performed. For suspected food allergies, medically supervised food challenges might be necessary for a definitive diagnosis.
Measuring fractional exhaled nitric oxide (FeNO) can help assess airway inflammation in asthma3. Discussing your history and symptoms with a doctor is vital for accurate identification and management planning.
Diagnosis and Getting Help
If you suspect you have allergies or asthma, getting a proper diagnosis from a qualified healthcare professional is essential. Self-diagnosing can lead to incorrect treatment, delayed care, or unnecessary avoidance measures. A healthcare professional, possibly specializing in allergy and clinical immunology, can provide an accurate assessment and guide treatment.
Do not hesitate to talk to your doctor about your symptoms, even if they seem mild. Early diagnosis and intervention can prevent complications and improve long-term outcomes. It helps you gain control over your condition sooner, leading to better overall health and well-being within the medical community.
Diagnosing Allergies
Diagnosing allergies usually starts with a thorough review of your medical history and a detailed discussion of your symptoms. Your doctor will ask about potential exposures, the timing and nature of your reactions, family history of allergies, and factors that seem to improve or worsen your symptoms.
A physical examination, looking for signs like nasal swelling, skin rashes, or wheezing, can also provide clues. To confirm the diagnosis and identify specific allergens, your doctor will likely suggest allergy testing. As mentioned, skin tests (skin prick testing, intradermal skin testing) and blood tests (specific IgE tests) are the standard methods for identifying sensitivities to inhaled allergens, foods, insect venom, and some medications.
Patch testing is specifically used for diagnosing contact dermatitis from chemicals or metals. These diagnostic tools are critical to develop an effective plan to treat allergies.
Diagnosing Asthma
Asthma diagnosis also involves looking carefully at your medical history and symptom patterns.
Your doctor will ask if you have a cough, especially at night. They will also check for wheezing, shortness of breath, and chest tightness. They will want to know how often these symptoms happen and how severe they are. They’ll also ask what triggers them, like exercise, colds, or allergens.
A physical exam is part of the process. The doctor will listen to your lungs with a stethoscope. Lung sounds can be normal between asthma attacks.
Lung function tests, especially spirometry, help confirm asthma. Spirometry checks how much air you can breathe in and out. It also measures how quickly you can exhale forcefully. The National Heart, Lung, and Blood Institute says that less airflow after using a bronchodilator means asthma. Measuring nitric oxide in your breath can reveal airway inflammation from asthma.
Finding the Right Specialist
Your primary care doctor can handle mild allergies or asthma. However, a specialist may offer more focused help. Allergists are board-certified in Allergy & Immunology. They often train in internal medicine or pediatrics first. These experts diagnose and treat allergies, asthma, and related immune issues. They perform and interpret allergy tests, like skin and patch testing. They identify complex triggers and suggest advanced treatments, such as immunotherapy.
Pulmonologists are lung specialists. They focus on respiratory diseases, especially severe asthma. Your main doctor might send you to a specialist. This usually depends on your needs and how complex your condition is. Good allergy and asthma care often requires teamwork. This may include your primary doctor, specialists, nurses, and pharmacists nearby4.
Many practices offer patient resources and online resources for support.
Effective Allergy and Asthma Care Strategies
After diagnosis, managing allergies and asthma requires a mix of strategies that suit you.
This often means:
- avoiding triggers
- taking your medicine as directed
- having a clear plan
Work closely with your doctor or allergy specialist. This helps you create and adjust your approach. Your plan should reflect your specific triggers, symptom type and severity, and lifestyle. Regular follow-ups help monitor your condition and adjust the plan as needed. Following your plan is essential for managing symptoms and reaching good health.
Allergen Avoidance
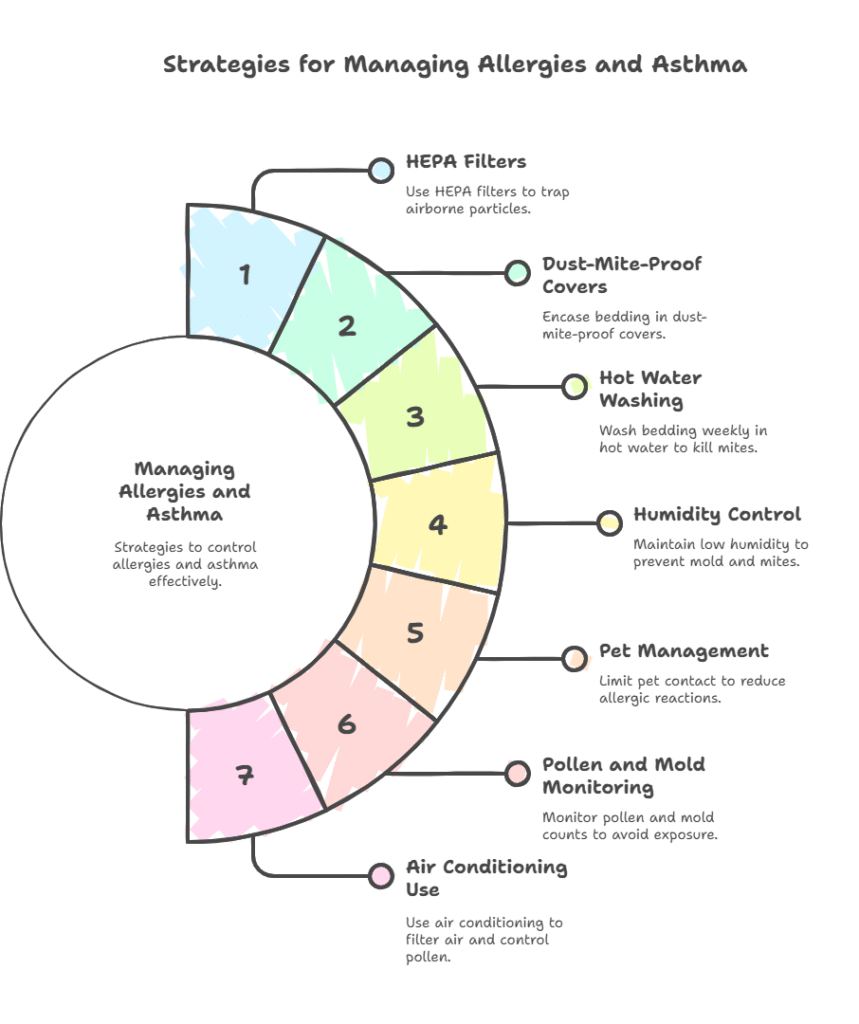
Reducing your exposure to allergens is key to managing allergies and asthma. Avoiding airborne allergens like pollen is tough. But reducing exposure can help. Understanding your triggers and taking steps to limit exposure is crucial. Here are some practical tips:
- Use HEPA filters in your home’s vents and vacuum to trap airborne particles.
- Encase pillows, mattresses, and box springs in dust-mite-proof covers.
- Wash bedding, like blankets and mattress pads, every week in hot water. Use water that’s at least 130°F (54°C). Then, dry them on high heat to kill dust mites.
- Keep indoor humidity low, ideally between 30-50%. Use dehumidifiers and air conditioning, especially in damp areas like basements. This helps prevent mold and dust mites.
- Limit contact with pets if you’re allergic. Keep them out of the bedroom and off furniture, and wash your hands after handling them.
- Check daily pollen and mold counts from local weather reports or online. Stay indoors with windows closed during peak times, especially on windy days.
- Use air conditioning at home and in your car. Don’t open windows when pollen levels are high.
Medications for Allergies
Several types of medications can help control allergy symptoms effectively.
Antihistamines are commonly used. They block histamine, a chemical released during allergic reactions. These come in pills, liquids, nasal sprays, and eye drops. Decongestants help ease a stuffy nose by narrowing blood vessels. However, use them only for short periods. Long-term use can cause side effects and rebound congestion5.
Nasal corticosteroids are effective anti-inflammatory sprays. They lower nasal inflammation, congestion, sneezing, and itching from allergic rhinitis (hay fever). Leukotriene modifiers are oral medications that block other chemicals involved in allergic reactions. They are sometimes used for allergies and asthma.
For moderate to severe allergies not managed by these medications, consider allergy shots or sublingual immunotherapy. Allergy shots are injections.
Sublingual immunotherapy comes as tablets or drops you place under your tongue. These treatments can slowly help the body get used to allergens. This includes pollen, dust mites, pet dander, and insect venom. The process takes several years.
Consulting with your provider helps determine the best treatment allergy approach.
Medications for Asthma
Asthma medications are mainly in two categories: quick-relief (rescue) and long-term control (maintenance).
Quick-relief inhalers, like albuterol, contain short-acting beta-agonists (SABAs). They quickly relax tight airway muscles. This helps open narrowed airways during an asthma attack. These inhalers are used as needed.
Long-term control medications are taken daily, even when feeling fine. They help stop symptoms. They reduce airway inflammation. They also lower how often and how severe asthma attacks are. Inhaled corticosteroids (ICS) are the mainstay for long-term asthma treatment. They are the most effective at reducing inflammation.
Combination inhalers include both an ICS and a long-acting beta-agonist (LABA). This provides both anti-inflammatory effects and longer airway relaxation.
Other control options include:
- Leukotriene modifiers (oral pills)
- Long-acting muscarinic antagonists (LAMAs)
- Biologics
Biologics are injectable medications for moderate to severe asthma. They target specific inflammatory cells or proteins. This includes IgE antibodies and eosinophils. These elements also contribute to conditions like eosinophilic esophagitis.
Learning the right inhaler technique is crucial. It helps ensure medications reach the lungs effectively. Ask your medical staff or pharmacist for a demonstration. Sometimes, hospitals use rapid desensitization protocols. They do this for critical medication needs when a drug allergy is present.
Developing an Asthma Action Plan
An Asthma Action Plan is a personal document made with your doctor. It guides you on managing asthma daily and tells you what to do during an attack. This plan helps you and your family take charge of the condition. It usually includes:
- A list of your daily medications and how to use them.
- Tips on spotting worsening symptoms, often using a zone system (Green, Yellow, Red) based on peak flow readings or symptom severity.
- Directions on which quick-relief medications to use and how often during flare-ups (Yellow Zone).
- Instructions on when to increase controller medications as your doctor advises.
- Criteria for when to seek immediate help or go to the emergency room (Red Zone).
Share this plan with family, school staff, and workplace supervisors. This helps everyone give consistent asthma care. Review and update the plan with your doctor regularly.
Do this at least once a year or whenever treatment changes. Many clinics offer a patient portal. This gives you access to medical records and communication tools.s, is also essential. Many clinics offer access to medical records and communication tools via a patient portal.
Lifestyle Adjustments for Better Control
Besides medications and steering clear of triggers, some habits can help control your allergies and asthma. Small, consistent changes in your daily routine can improve how you feel and breathe.
These adjustments aim to boost your health and lower exposure to respiratory irritants. It’s important to think about how diet, exercise, stress, and your home affect your breathing. Making healthy choices in these areas can support your medical treatment. Talk to your doctor or allergy specialist before making any big lifestyle changes.
Healthy Eating
Diet isn’t usually seen as a direct cure for allergies or asthma. However, eating well boosts overall health and strengthens immunity. Some studies show that diets rich in fruits and vegetables can lower inflammation. Antioxidants, like vitamins C and E, also help. Omega-3 fatty acids, found in fatty fish, may also aid in managing chronic inflammation.
Be aware of food sensitivities or allergies that allergy tests reveal. If you have food allergies, it’s important to avoid trigger foods. This helps prevent reactions. Read food labels carefully. Know hidden ingredients. Always tell others about your allergies when you eat out.
A balanced diet enhances physical resilience and well-being. This can indirectly help your body manage chronic issues like allergies and asthma.
Staying Active with Asthma
Having asthma doesn’t mean you must stop exercising. Regular, moderate activity can strengthen your lungs and improve your heart health. It can also help you maintain a healthy weight and boost your quality of life. The key is to exercise safely and smartly while managing any symptoms.
Talk to your doctor or an asthma specialist at your clinic. They can suggest the best activities for you and how to manage your asthma during exercise. Always start with a gradual warm-up and end with a cool-down. This helps your airways adjust to activity.
If your doctor recommends it, use your quick-relief inhaler 15-30 minutes before exercising. This can help prevent exercise-induced bronchoconstriction (EIB). Stay indoors when pollen or pollution is high if it affects your asthma.
Be careful when exercising in very cold, dry air. A scarf or mask over your mouth and nose can warm and humidify the air you breathe. With the right management, most people with asthma can enjoy sports and activities.
Managing Stress
Stress doesn’t cause asthma or allergies directly. But for some people, it can make symptoms worse. When you’re stressed, your body releases hormones and chemicals. These include cortisol and histamine. These can increase inflammation in your body, including your airways.
Finding healthy ways to cope with daily stress is good for your mental and physical health. Techniques such as mindfulness meditation, deep breathing, and progressive muscle relaxation can help. Yoga and tai chi are also effective for reducing stress and promoting calmness.
Spending time in nature is important. So is enjoying hobbies and getting enough restful sleep. Find what eases your stress. Then, add those activities to your routine. This can help improve your emotional balance and may reduce symptom flare-ups.
Creating a Healthier Home Environment
Your home should be a safe haven, but hidden allergens can trigger allergy or asthma symptoms. You can improve indoor air quality and reduce exposure to common triggers.
This is key for managing symptoms daily. You need more than just occasional cleaning. Consistent effort is key, and you should focus on known triggers. Here is a table summarizing key actions for a healthier home:
| Area | Action | Benefit |
|---|---|---|
| Air Quality | Use HEPA air purifiers in main living areas and bedrooms; change HVAC filters regularly with high-quality filters. | Reduces airborne allergens like pollen, dust mite debris, pet dander, and mold spores. |
| Bedrooms | Encase pillows, mattresses, and box springs in allergen-impermeable covers; wash all bedding in hot water weekly. | Minimizes exposure to dust mites, a common trigger, during sleep. |
| Cleaning | Vacuum frequently (once or twice weekly) using a vacuum cleaner with a HEPA filter; damp mop hard floors instead of sweeping. Use microfiber cloths for dusting. | Removes surface dust and allergens effectively without stirring them back into the air. |
| Humidity | Keep indoor humidity levels ideally between 30-50% using dehumidifiers in damp areas and ensuring good ventilation, especially in bathrooms and kitchens. | Discourages the growth of mold and reduces populations of dust mites. |
| Pets | If pet allergy is confirmed, ideally keep pets out of the home, or at minimum, strictly out of bedrooms; wash hands and change clothes after significant pet contact. Consider HEPA filters. | Lowers exposure levels to pet dander and other animal allergens. |
| Smoking | Maintain a strictly smoke-free home and car environment at all times. Avoid exposure to secondhand smoke outside the home as well. | Eliminates a major respiratory irritant and a significant trigger for asthma attacks and worsening symptoms. |
| Chemicals & Scents | Choose fragrance-free cleaning products and personal care items; ensure good ventilation when using strong chemicals. Avoid using strong air fresheners or scented candles. | Reduces exposure to irritants that can trigger asthma or allergy symptoms. |
Making these changes can lead to a more comfortable living space. A clean, low-allergen home is key for managing your allergies and asthma.
Small, regular steps can create big changes. They help manage symptoms and boost well-being. Remember to check office hours for appointments or allergy shots.
Many offices shut down for big holidays. These include Memorial Day, Labor Day, and Independence Day. Use patient forms and the patient portal from your clinic for convenience. The office and medical staff are there to help. Many patients recommend specific clinics based on their positive experiences.
Conclusion
Living with allergies and asthma takes effort and awareness. Understanding your conditions is key. Sticking to your management plan helps a lot. Avoiding triggers can make your daily life better. Good allergy and asthma care is possible, helping you live a healthier, more active life.
Work closely with your healthcare providers. Speak freely with your primary care doctor and specialists like allergists or pulmonologists. They will help you create a treatment plan that fits your needs, symptoms, and lifestyle goals.
You can manage your symptoms by mixing avoidance strategies, medications, and immunotherapy. These include allergy shots and oral immunotherapy. This lets you breathe easier and enjoy life despite these common chronic conditions. Taking charge of your allergy and asthma care can boost your health and well-being.
Small Step, Big Impact
To effectively manage allergies and asthma, start by identifying your specific triggers, consult with healthcare professionals for personalized treatment plans, and implement daily preventive measures to reduce exposure and symptoms.
Listen to this article
This is an AI generated Podcast version of the article.
- https://aafa.org/allergies/prevent-allergies/control-indoor-allergens/[↩]
- https://my.clevelandclinic.org/health/diagnostics/21495-allergy-testing[↩]
- https://pmc.ncbi.nlm.nih.gov/articles/PMC6690504/[↩]
- https://www.lung.org/blog/know-your-providers-pulmonologist[↩]
- https://www.webmd.com/allergies/antihistamines-1[↩]



